The CPM Tool has been developed to help NHS organisations redesign services to enhance the management and care of patients with chronic pain within a local health economy whilst reducing inappropriate practice prescribing. The CPM Tool has been created by Helping Health Ltd, based on the doctoral research of Dr Cathy Alexander (Helping Health Director).
What are the consequences of not improving local chronic pain management?
Prescribing of opioids has increased significantly in the UK over the past thirty years and has now become the largest reported opioid using population in Europe. Whilst opioids are effective against acute pain, the significant increase in levels of prescribing of opioids can be attributed to treatments relating to chronic pain (CP). Patients receiving opioids for chronic pain develop addiction and suffer debilitating withdrawal symptoms with limited evidence of clinical benefit from the medication. Chronic pain, often associated with musculoskeletal conditions, is a significant issue strongly linked to advancing age. Given the UK’s aging population, the prevalence of patients experiencing chronic pain will continue to rise, which if left unaddressed, will exacerbate the current problem. At a more localised level, chronic pain treatment and prescribing vary greatly across England with little or no association between expenditure and outcomes, reflecting a fragmented approach. This was the catalyst for development of the CPM Tool, which aims to improve patient outcomes while reducing costs for the NHS.
What is the CPM?
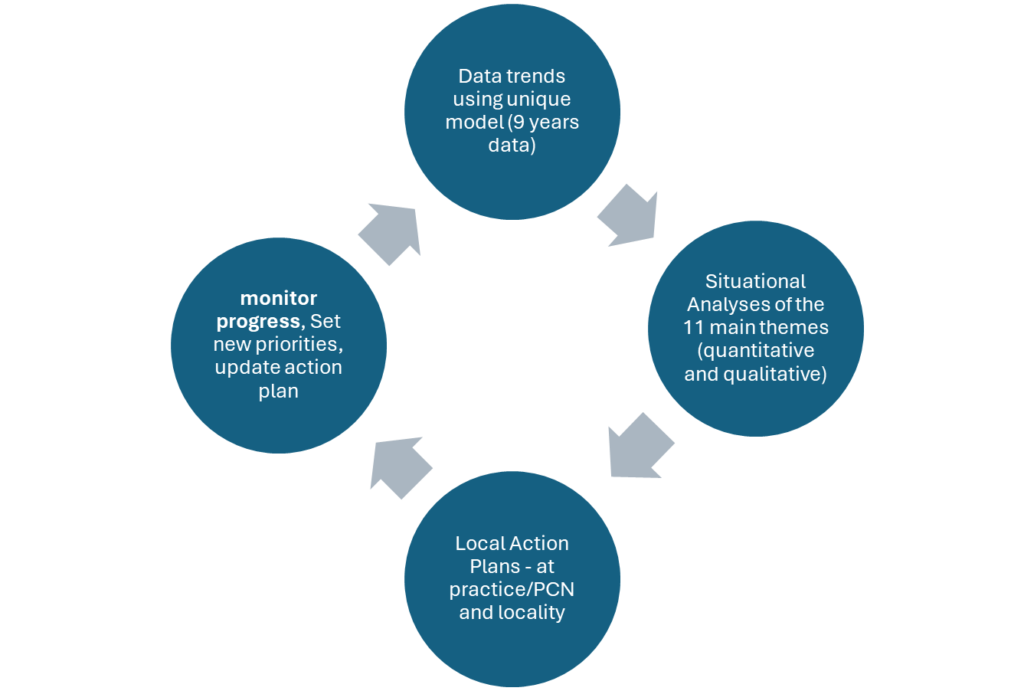
The CPM Tool is a web-based programme, which is built upon a comprehensive database covering all GP practices in England. It takes large amounts of NHS quantitative data, qualitative information from bespoke questionnaires and additional intelligence from discussions with stakeholders to create locally specific action plans at practice/primary care network and locality levels. Outcomes are set and progress monitored throughout the year.
The CPM contains data trends for all practices in England and allows the user full autonomy to compare across the whole of England which is invaluable in revealing how the local situation contrasts with other areas. There are 11 groups of factors and over 50 individual datasets:
- Patient and Population Need
- Resources available
- Management and referrals of pain locally
- Alternative ways of managing pain
- Organisation culture and management
- Influence of other organisations
- Opioid prescribing rates
- Prescribing rates of alternatives to opioids
- Patient involvement
- Medicines Optimisation
- General Prescribing behaviour
This is a unique approach which uses a model to link data and local insight to form bespoke practice and locality action plans.
Why use the CPM Tool?
The CPM Tool changes the way chronic pain is managed within the local health economy by moving the focus away from prescribing of dependence forming drugs and complex surgical interventions in acute care. Instead, it encourages chronic pain patients to adopt healthy behaviour (keeping active, improving mental health, increasing social interactions and linking up with other patients). This is in line with national guidance and frameworks1,2,3,4,5,6 for better management of pain. The CPM Tool will help NHS organisations achieve government targets as well as embed changes in behaviour to improve management of chronic pain.
Using the CPM Tool

Summary
Using the CPM Tool, NHS organisations are able to:
- Improve the quality of life of people who have chronic pain.
- Improve the effectiveness of care for people with chronic pain
- Improve the equity of care for people with chronic pain
- Improve the cost effectiveness of care
- Reduce inappropriate prescribing of dependence forming drugs for people with chronic pain
References:
1NHS ENGLAND 2023. Optimising personalised care for adults prescribed medicines associated with dependence or withdrawal symptoms: Framework for action for integrated care boards (ICBs) and primary care 14/03/2023, 15:17 Date published: 2 March 2023 Date last updated: 7 March 2023
2NICE 2022. Osteoarthritis in over 16s: diagnosis and management. NICE guideline NG226. Published 19 October 2022
3NICE 2021 (a) Chronic Pain (Primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain [J] Evidence review for pharmacological management of chronic primary pain NICE Guideline NG193. Intervention evidence review underpinning recommendations 1.2.7 to 1.2.15 and the research recommendation in the NICE guideline. April 2021 ISBN 978-1-4731-4066-0.
4NICE 2021 (b) Resource impact report: Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain (NG193) April 2021.
5NICE 2019.Medicines Optimisation in Chronic Pain. Key therapeutic topic [KTT21]. Published date: 16 January 2017 Last updated: 01 September 2019.
6NICE 2017. National Low Back and Radicular Pain Pathway 2017 including implementation of NICE Guidance NG59. Third Edition 3.0. 30 June 2017
For more information or a demonstration of the tool, please contact us on 01823 321211